Acid Reflux, or Heartburn…
If you’ve ever experienced it, you’ll be familiar with the experience of burning chest pain from stomach acid moving up into the oesophagus and irritating its delicate lining.
It seems to make sense that if you feel acid moving from your stomach into your oesophagus that you must have “too much” acid, spilling up and out right? But actually, it can more often than not be the reverse.
Any amount of acid moving from the safety of the gut (where it likes to be acidic to digest your last meal) into an area not built for handling an acidic environment will cause this burning (not just that there’s “too much” acid). So if it’s not too much acid, what is giving you that awful feeling?
Intra-Abdominal Pressure and the LES
The only way acid can move back from the stomach into the oesophagus is via the Lower Oesophageal Sphincter (LES). This valve should allow food down the oesophagus into the stomach and keep stomach acid where it belongs. Reflux can occur when the valve itself is faulty and allows acid to flow backwards.
A common cause for a faulty valve is an increase in intra-abdominal pressure.
So how does that happen?
Well it can occur when we get an increase in intestinal bacteria (or what’s known as intestinal bacterial overgrowth) and/or we experience carbohydrate malabsorption. (OK, let’s keep playing this game…)
And how do you get intestinal bacterial overgrowth and/or carb malabsorption?
Well that would be from low stomach acid.
Low Stomach Acid (or Hypochlorhydria)
As we age, our stomach acid declines, yet the incidence of GORD (gastro-oesophageal reflux disease) increases.
When we carefully test people over age forty who’re having heartburn, indigestion and gas, over 90 percent of the time we find inadequate acid production by the stomach.
Dr. Natasha Campbell-McBride, creator of the Gut and Psychology Syndrome (GAPS) diet also links poor gut health and inadequate gut flora with low stomach acid:
Toxins produced by overgrowth of Candida species, Clostridia and other pathogens have a strong ability to reduce secretion of stomach acid.
Help!
So what can you do before reaching for the Gaviscon or Proton Pump Inhibitor?
The solution could be an anti-antacid: i.e. increasing hydrochloric acid (or Betain HCl):
In 24 years of nutritionally oriented practice, I’ve worked with thousands of individuals who’ve found the cause of their heartburn and indigestion to be low stomach acidity. In nearly all these folks, symptoms have been relieved and digestion improved when they’ve taken supplemental hydrochloric acid and pepsin capsules.
Diet
Choose a wholefood diet (avoiding gluten grains if suspected sensitivity) or investigate The Body Ecology Diet or GAPS Diet.
5 Foods That May Help
Pineapple and Papaya
The active ingredients in pineapple and papaya, bromelain + quercetain, are anti-inflammatory and anti-oxidant. In particular, bromelain is important for protein digestion (proteolytic enzyme) which may be lacking in cases of low HCl.
Oysters/fish/seeds
A good source of zinc. With low stomach acid, zinc levels may be compromised and zinc is required for the production of HCl, multiple enzymes within the GIT and an overall healthy immune response.
Bitter greens
Rocket, radicchio; and bitter drinks pre-meal: lemon juice or apple cider vinegar (incl mother) in warm water before meals: via taste receptors on the tongue, increases saliva, gastrin and HCl within the stomach to maximise digestion.
Probiotic foods
Sauerkraut or yoghurts containing Bifidobacteria and Lactobacillus spp. may improve mucosa lining damage and maintain healthy gut flora.
Ginger (tea/foods)
Aids digestion, is warming and may reduce bloating.
5 Foods to Avoid
Gluten grains (wheat, rye, barley)
If sensitive, gluten may exacerbate inflammation of already compromised GIT via mucosa weakness and/or pathogens within gut.
Sugar
Encourages growth of yeasts such as Candida spp. which may already be prolific in an under-acidic environment.
Alcohol (Beer)
High yeast/sugar content may encourage overgrowth of Candida spp.
Bread/pasta
Reduces gut motility.
Cheese
Reduces gut motility.
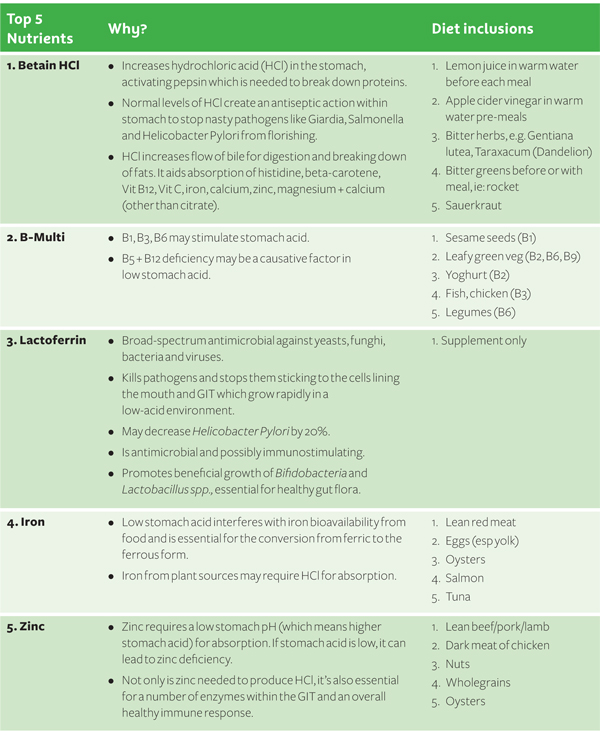
I Prefer a Table!
Well here you go.
References
- GAPS Australia, Betain HCL Pepsin or Sauerkraut: FOUR.: Digestive Enzymes, http://gapsaustralia.com.au/betain-hcl-pepsin-or-sauerkraut/?doing_wp_cron=1401742198.7018818855285644531250
- Hechtman L 2011, Clinical naturopathic medicine, Elsevier, Chatswood NSW
Kelly G 1997, ‘Hydrochloric Acid: Physiological Functions And Clinical Implications,’ Alt Med Review, 2:(2):116-127 - Kennedy R 2011, Hypochlorhydria, The Doctor’s Medical Library, CA, viewed 27 Feb 2012, http://www.medical-library.net/hypochlorhydria.html
- Kresser C, What Everybody Ought To Know (But Doesn’t) About Heartburn & GERD, viewed 3 June 2014,http://chriskresser.com/what-everybody-ought-to-know-but-doesnt-about-heartburn-gerd
- Pizzorno J et. al. 2008, The clinician’s handbook of natural medicine, 2nd edition, Churchill Livingstone Elsevier, Missouri
- The Food Doctor 2012, Bloating, UK, viewed 27 Feb 2012, http://www.thefooddoctor.com/Bloating-Ahealth_fdw_bloat/
- Thomsen & Gennat 2009, Phytotherapy desk reference, 4th edition, Global Natural Medicine, Australia
Kate is a qualified naturopath who is passionate about helping women heal from hormonal havoc and inspiring women to know their own power, worth and wisdom.
Kate offers one-on-one Skype consults for irregular cycles, PMS and period pain, endometriosis, PCOS, peri-menopause, mood swings, fatigue and mental and emotional stress.
Simply drop me an email to see how I can help you!